Need Cialis through Tricare? Begin by contacting your Tricare provider. Confirm your prescription coverage and understand the specific requirements for prior authorization. This often involves providing detailed medical information supporting the necessity of Cialis for your condition.
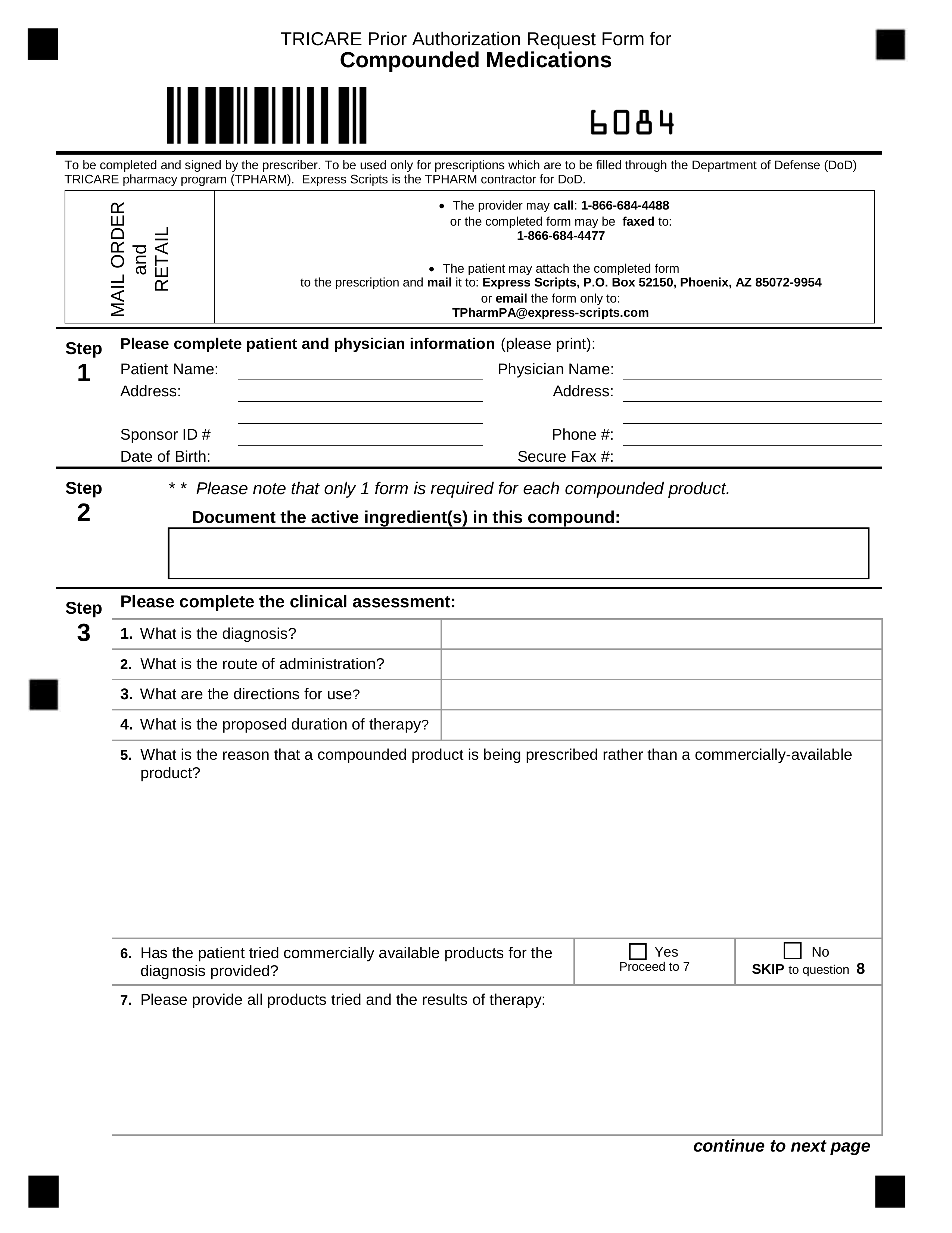
Gather all necessary documentation. This typically includes a completed prior authorization form, your doctor’s prescription, and medical records detailing your diagnosis and treatment history. Accurate and complete documentation significantly speeds up the process. Failure to submit all required documents will likely delay approval.
Expect the review process to take several days, sometimes longer. Follow up with your Tricare provider if you haven’t received a decision within a reasonable timeframe, proactively managing the process ensures a quicker resolution. Remember to retain copies of all submitted documents for your records.
Pro Tip: Direct communication with your doctor and Tricare is key. Clarify any ambiguities early on to prevent delays. Understanding your coverage limits and potential out-of-pocket costs beforehand helps manage expectations.
Disclaimer: This information is for guidance only and does not constitute medical advice. Always consult your healthcare provider and Tricare for the most current and accurate information.
- Tricare Prior Authorization for Cialis: A Detailed Guide
- Understanding Tricare’s Requirements
- Gathering Necessary Documentation
- The Tricare Prior Authorization Form
- Expected Processing Time
- Appealing a Denied Request
- Comparison of Tricare Plans and Cialis Coverage
- Contacting Tricare Directly
- Understanding Tricare’s Prior Authorization Process
- Specific Requirements for Cialis Prior Authorization
- Gathering Necessary Documentation for Your Claim
- Medical Records and Supporting Documentation
- Your Tricare Information
- Submitting Your Prior Authorization Request to Tricare
- Using the Online Portal
- Submitting by Mail
- Contacting Tricare
- Tracking Your Prior Authorization Request and Appeal Options
- Using the Tricare Website and Phone
- Understanding the Appeal Process
- Appeal Steps
- Additional Resources
- Timeframes
- Understanding Potential Delays and Denials
Tricare Prior Authorization for Cialis: A Detailed Guide
Begin by contacting your Tricare provider. They can verify your coverage and explain the specific requirements for prior authorization.
Understanding Tricare’s Requirements
Tricare generally requires prior authorization for Cialis when prescribed for erectile dysfunction. The specific requirements can vary based on your Tricare plan (Prime, Select, Reserve Select, etc.). Expect to provide detailed medical information, including your medical history and current medications. Your physician will need to submit a completed prior authorization form outlining the medical necessity of Cialis for your condition.
Gathering Necessary Documentation
To streamline the process, ensure your doctor provides all necessary documentation. This typically includes: a completed Tricare prior authorization form, a detailed explanation of your medical condition, and documentation supporting the need for Cialis. Incomplete submissions often lead to delays.
The Tricare Prior Authorization Form
This form requires specific information, including your personal details, diagnosis, treatment plan, and justification for Cialis. Ensure all fields are accurately completed; inaccuracies can cause delays or rejection. Download the form directly from the Tricare website; ensure you’re using the most up-to-date version.
Expected Processing Time
Processing times vary. Expect a response within several weeks. Follow up if you haven’t heard back within the expected timeframe.
Appealing a Denied Request
If your prior authorization is denied, review the denial reason carefully. You or your physician can submit an appeal with additional supporting medical documentation. Understand the appeal process detailed in your Tricare plan materials.
Comparison of Tricare Plans and Cialis Coverage
| Tricare Plan | Cialis Coverage (with prior authorization) | Notes |
|---|---|---|
| Tricare Prime | Generally covered | Coverage specifics depend on your specific pharmacy and doctor. |
| Tricare Select | Generally covered | Higher cost-sharing compared to Prime. |
| Tricare Reserve Select | Generally covered | Similar to Select, but with different cost-sharing details. |
Contacting Tricare Directly
If you experience difficulties or have questions, contact Tricare directly via phone or their website. Their customer service representatives can provide specific guidance regarding your situation and plan.
Understanding Tricare’s Prior Authorization Process
Check your Tricare plan’s formulary first. This will tell you if Cialis requires prior authorization.
If prior authorization is needed, gather these documents:
- Your doctor’s prescription
- Your doctor’s completed Tricare prior authorization form (available online or from your doctor)
- Medical records supporting your need for Cialis. This might include lab results or notes detailing your condition.
Submit your paperwork to the correct Tricare contractor. You can find contact information on the Tricare website, usually specific to your region.
Expect a decision within a specific timeframe; this varies depending on your plan and the contractor’s processing time. Check the Tricare website for typical processing times.
If your prior authorization is denied, understand your appeal rights. Tricare offers formal processes for appeal. Follow the instructions provided in the denial letter carefully; these often explain the next steps.
- Review the denial reason. This helps tailor your appeal. Did the doctor’s documentation lack key details?
- Gather additional information to support your appeal. This might include updated medical records, a new physician’s letter, or alternative treatment options.
- Submit a detailed appeal following Tricare’s instructions. Clearly state the reason for the appeal, referencing the denial and providing the requested supporting documentation.
If you experience difficulties, contact Tricare directly. They provide support lines for beneficiaries. Your Tricare provider can also assist in navigating the process.
Specific Requirements for Cialis Prior Authorization
To obtain Tricare prior authorization for Cialis, ensure your prescription is for erectile dysfunction. The prescribing physician must submit a completed prior authorization form, including detailed patient medical history documenting the diagnosis and treatment attempts.
Include specific details on failed alternative treatments, such as PDE5 inhibitors other than Tadalafil (Cialis), and any relevant comorbidities that may impact treatment choice. Clearly state the dosage and frequency requested.
The form requires the physician’s signature and contact information. Incomplete forms often lead to delays. Upload all supporting documentation, such as lab results and physician notes, directly through the Tricare portal or as directed by the submission guidelines.
Check the Tricare website regularly for any updates to their prior authorization requirements. These requirements are subject to change, and timely updates are crucial for a smooth process.
If your claim is denied, carefully review the denial letter and identify areas needing improvement. Contact Tricare directly to clarify any uncertainties and discuss options for resubmission.
Prior authorization often takes several business days for processing; allow ample time before your needed refill date.
Gathering Necessary Documentation for Your Claim
Begin by collecting your prescription information: the date it was written, the dosage, and the quantity prescribed. Include your physician’s contact details – name, address, phone number, and fax number. A copy of your prescription itself is also necessary.
Medical Records and Supporting Documentation
Provide any relevant medical records supporting the need for Cialis. This could include doctor’s notes detailing your diagnosis, prior treatments, and their effectiveness (or lack thereof). Diagnostic test results, such as blood work or imaging reports, are also helpful. Finally, submit any documentation outlining prior attempts at alternative treatments.
Your Tricare Information
Ensure your claim includes your full name, your Tricare ID number, and your current mailing address. Accurate and complete information expedites the processing of your request. If you have a sponsor, provide their information as well.
Submit all documentation together. Carefully review the Tricare website for the most up-to-date requirements and submission guidelines. Contact Tricare directly if you have any questions regarding specific documents required for your situation.
Submitting Your Prior Authorization Request to Tricare
Gather all necessary documentation: your prescription, doctor’s notes supporting medical necessity, and your Tricare ID card. Clearly label each document with your name and date of birth.
Download the correct Prior Authorization form from the Tricare website. Ensure you use the most up-to-date version. Carefully complete all sections; inaccurate information delays processing.
Using the Online Portal
Submit your request through the Tricare online portal for faster processing. This method provides tracking capabilities, allowing you to monitor your request’s status. Log in using your secure credentials and follow the instructions for prior authorization submission.
Submitting by Mail
If using mail, send your completed form and supporting documents via certified mail with return receipt requested. This provides proof of delivery and helps ensure your request reaches the appropriate Tricare office. Address your request to the Tricare contractor responsible for your region, as outlined on your Tricare ID card or the Tricare website.
Contacting Tricare
After submitting, allow the processing time indicated on the Tricare website. If you have questions or if your request has not been processed within the expected timeframe, contact Tricare customer service using the phone number or email address found on their website.
Tracking Your Prior Authorization Request and Appeal Options
Check your Tricare provider’s online portal regularly. Most offer a secure patient portal where you can monitor your request status. Expect updates on the progress of your prior authorization.
Using the Tricare Website and Phone
The Tricare website provides tools to track your request. You’ll find instructions and frequently asked questions. Use the contact information provided to reach Tricare directly if you have questions.
- Phone: Call the Tricare number for your region.
- Website: Access your online account to check your request status, using your member ID.
Understanding the Appeal Process
If your prior authorization is denied, you have the right to appeal. Gather all relevant medical documentation, such as doctor’s notes and test results. This strengthens your appeal.
Appeal Steps
- Review the denial: Carefully read the denial letter to understand the reasons for rejection.
- Prepare your appeal: Include all supporting medical records and a clear explanation of why you believe the medication is medically necessary.
- Submit your appeal: Follow the instructions in your denial letter for submitting the appeal. Use certified mail for proof of submission.
- Track your appeal: Follow up on the status of your appeal using the same methods as you did with your prior authorization.
Additional Resources
Tricare offers a wealth of information online. Explore their FAQs and member handbooks for detailed guidelines. Consider consulting with your doctor or a Tricare representative.
Timeframes
Keep track of deadlines for both your prior authorization and any appeals. Late submissions may negatively affect your case.
Understanding Potential Delays and Denials
Check your prescription details meticulously against Tricare’s formulary. Incorrect information leads to immediate rejection.
Ensure your doctor submits all required documentation. Missing forms significantly increase processing time. Specifically, review Tricare’s website for the complete list of needed forms for Cialis prior authorization.
Confirm your provider’s participation in the Tricare network. Out-of-network providers may face additional hurdles in getting authorizations approved.
Understand Tricare’s criteria for Cialis approval. Conditions such as benign prostatic hyperplasia (BPH) or erectile dysfunction (ED) must be clearly documented. Incomplete medical justifications frequently cause denial.
Allow ample processing time. Typical wait times vary, but expect several business days, possibly longer during peak periods. Follow up directly with Tricare if you experience unusual delays.
If your prior authorization is denied, immediately request a detailed explanation. This explanation outlines reasons for denial and suggests steps to correct the application. Appeal the decision if you disagree with Tricare’s assessment.
Consider contacting Tricare’s customer service for assistance. Their representatives can provide clarification and guidance during the process.