Need Cialis but facing prior authorization hurdles? Contact your insurance provider immediately to understand their specific requirements. Confirm if they require pre-authorization for Cialis, and if so, gather all necessary documentation upfront.
Typically, this includes your doctor’s prescription, your insurance card details, and possibly medical records relevant to your condition. Proactively submitting a complete application significantly reduces processing time. Expect a response within a few business days, but delays are possible. Therefore, plan ahead and don’t wait until the last minute to initiate the process.
If your initial application is denied, don’t despair. Review the denial letter carefully; it often outlines reasons for rejection and suggests steps to remedy the situation. You might need to provide additional medical information or consider alternative treatment options in consultation with your physician. Appealing a denial is often possible, following the insurer’s outlined procedures.
Remember: Your doctor can play a key role in navigating this process. They can help gather necessary information, advocate on your behalf with your insurance company, and explore alternative treatment pathways if needed. Open communication is key to a successful outcome.
- Cialis Prior Authorization: A Comprehensive Guide
- Understanding Your Insurance Plan
- Submitting Your Prior Authorization Request
- Appealing a Denied Request
- What is Prior Authorization for Cialis?
- Why Does My Insurance Require Prior Authorization?
- What Happens During the Prior Authorization Process?
- What Information Will My Doctor Need?
- What If My Prior Authorization is Denied?
- Helpful Tips for a Smooth Process
- Contacting Your Insurance Provider
- Common Reasons for Cialis Prior Authorization Requests
- Gathering Required Documentation for Your Cialis Prior Authorization
- Submitting Your Cialis Prior Authorization Request: A Step-by-Step Guide
- Understanding Potential Delays and Denials of Cialis Prior Authorization
- Common Reasons for Delays and Denials
- Steps to Minimize Delays
- Specific Documentation to Include
- Appealing a Denied Cialis Prior Authorization Request
- Alternative Medications and Cost-Saving Strategies If Cialis is Denied
- Other PDE5 Inhibitors
- Lifestyle Changes and Alternative Approaches
Cialis Prior Authorization: A Comprehensive Guide
Check your insurance plan’s formulary first. This lists covered medications and may indicate whether prior authorization (PA) is required for Cialis. Your plan’s website or member services line provides this information.
Understanding Your Insurance Plan
Contact your insurance provider directly. Ask specifically about Cialis PA requirements, including necessary documentation and the appeals process if your initial request is denied. Get the contact details of the PA department for faster processing.
Gather the required documents beforehand. This typically includes your prescription, doctor’s notes explaining the medical necessity of Cialis, and possibly prior treatment records. Having everything readily available expedites the process significantly.
Submitting Your Prior Authorization Request
Submit your PA request using your insurer’s preferred method – online portal, fax, or mail. Carefully follow all instructions to avoid delays. Use certified mail with tracking for the physical mail submission if required for proof of delivery. Note all relevant tracking details.
Follow up regularly after submission. Contact the PA department if you don’t receive an update within the expected timeframe provided by the insurer. Be polite and persistent, providing any required clarifications promptly.
Appealing a Denied Request
Review the denial letter carefully. Understand the reasons for denial. If you disagree, prepare a strong appeal. Provide additional supporting medical evidence if necessary. Your doctor might be able to help with this. Keep records of all communication during the appeals process.
Explore alternative options. If the appeal is denied again, discuss alternative treatments or medications with your doctor and consider a different insurance plan if feasible.
What is Prior Authorization for Cialis?
Prior authorization for Cialis means your insurance company requires your doctor to get pre-approval before covering the medication. This is a common process for many prescription drugs, including Cialis.
Why Does My Insurance Require Prior Authorization?
Insurance companies use prior authorization to manage costs and ensure appropriate medication use. They may require it because Cialis is a relatively expensive drug, or because there are other, cheaper treatments they prefer for your specific condition. They might also want to ensure the medication is medically necessary for you.
What Happens During the Prior Authorization Process?
Your doctor submits a request to your insurance company, providing information about your medical history and the reason Cialis is necessary. The insurance company reviews this information and decides whether to approve or deny coverage. This process can take several days, or even weeks.
What Information Will My Doctor Need?
Your doctor will need detailed information about your medical history, including any existing conditions, current medications, and previous treatments for erectile dysfunction. They’ll also need to explain why Cialis is the most appropriate medication for your situation and why alternatives are unsuitable.
What If My Prior Authorization is Denied?
If your prior authorization is denied, your doctor can appeal the decision by providing additional information to support the necessity of Cialis. Alternatively, you may explore alternative treatments covered by your insurance.
Helpful Tips for a Smooth Process
To make the process smoother, ensure your doctor has all the necessary information upfront. Contact your insurance provider directly to understand their specific requirements for prior authorization and required documentation.
| Step | Action |
|---|---|
| 1 | Doctor initiates prior authorization request. |
| 2 | Insurance company reviews the request. |
| 3 | Insurance company approves or denies the request. |
| 4 | If denied, appeal the decision or explore alternatives. |
Contacting Your Insurance Provider
Don’t hesitate to contact your insurance company directly. They can provide the most accurate and up-to-date information regarding their specific prior authorization procedures for Cialis. Having a clear understanding of their requirements can significantly simplify the process.
Common Reasons for Cialis Prior Authorization Requests
Prior authorization for Cialis often stems from specific factors your insurance company considers. Understanding these helps streamline the process.
- Prior Treatment Failure: Your insurer might require documentation showing other treatments for erectile dysfunction haven’t worked before approving Cialis.
- Diagnosis Verification: They may need confirmation of your erectile dysfunction diagnosis from your physician, including specific testing results. This ensures appropriate medication use.
- Alternative Treatments: Insurers frequently favor less expensive treatment options first. They may request attempts at lifestyle modifications or other medications before approving Cialis.
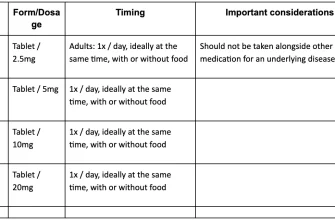
- Dosage and Duration: High doses or extended treatment periods might trigger prior authorization to prevent unnecessary expense or potential side effects.
- Contraindications: Certain health conditions can interact negatively with Cialis. Your doctor must demonstrate you don’t have these issues to obtain approval.
- Generic Alternatives: Your plan might prefer generic tadalafil. Providing evidence you can’t tolerate generic medication can support the Cialis request.
- Specialty Pharmacy Requirements: Some plans mandate Cialis dispensation through a specialty pharmacy. This involves additional steps, but is often a necessary part of obtaining coverage.
Proactively gather the necessary documentation, including medical records and test results, to expedite the process. Contact your insurance provider or pharmacist for specific requirements concerning your plan.
- Check your plan’s formulary for coverage details.
- Obtain required forms and instructions from your insurer.
- Provide complete and accurate medical information to your doctor.
- Follow up on the prior authorization request’s status.
Careful preparation can significantly shorten the wait time for authorization.
Gathering Required Documentation for Your Cialis Prior Authorization
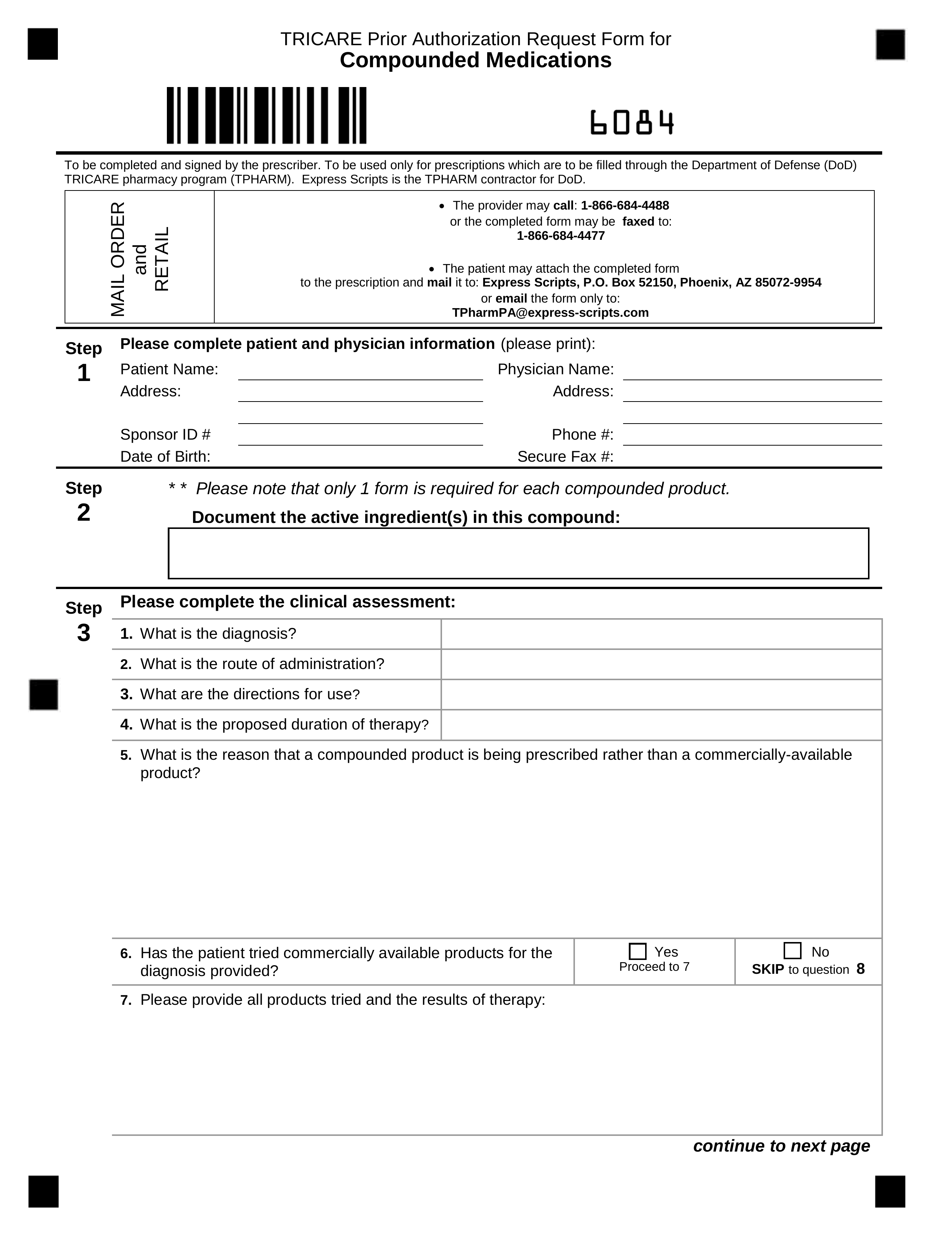
Begin by contacting your insurance provider. Obtain a complete list of required forms and supporting documents. This usually includes a prescription from your doctor.
Next, acquire your doctor’s completed and signed prior authorization form. Ensure all sections are filled accurately, including diagnoses, treatment plans, and relevant medical history. Inaccurate information can delay the approval process.
Your medical records may also be necessary. These support your doctor’s prescription and demonstrate the medical need for Cialis. Gather records related to your condition and previous treatments. Organize these documents chronologically for easy review.
If applicable, include any relevant lab results. These provide objective evidence supporting your diagnosis and the need for Cialis. Clearly label and date each document.
Finally, submit all documentation promptly via your insurance provider’s preferred method–mail, fax, or online portal. Keep copies of all submitted materials for your records.
Note: Specific requirements vary by insurance provider. Always consult your insurance plan’s details for precise instructions.
Pro Tip: Contact your doctor’s office for assistance in gathering necessary medical records. They can often expedite the process.
Submitting Your Cialis Prior Authorization Request: A Step-by-Step Guide
First, contact your insurance provider to obtain the necessary prior authorization forms. Download these forms directly from their website if available.
Next, carefully complete all sections of the form. Use black ink and print clearly. Include your patient information, prescription details (including dosage and quantity), and your doctor’s information. Be precise; inaccuracies delay processing.
Gather supporting medical documentation. This usually includes a copy of your prescription and a letter from your doctor explaining the medical necessity of Cialis for your specific condition. Ensure this letter explicitly states the diagnosis and why other treatment options were deemed unsuitable.
Once you’ve assembled all documents, submit your completed prior authorization request. Mail it via certified mail for confirmation of receipt or use the provider’s online portal if that option is available. Keep a copy for your records.
After submission, track your request’s status. Check the provider’s website or call their customer service line for updates. You may need to follow up after a reasonable timeframe if you haven’t received a response.
If your request is denied, understand the reasons for denial. Review the explanation carefully and consider appealing the decision. Your doctor can help navigate the appeal process and provide further medical justification.
Understanding Potential Delays and Denials of Cialis Prior Authorization
Prior authorization for Cialis can be delayed or denied for several reasons. Proactively addressing these issues can significantly speed up the process.
Common Reasons for Delays and Denials
- Incomplete Application: Missing information, such as diagnosis codes or patient details, frequently causes delays. Double-check all fields for accuracy before submission.
- Lack of Medical Necessity: Insurers require justification for Cialis use. Ensure your doctor’s documentation clearly demonstrates the medical necessity, citing specific symptoms and the failure of alternative treatments.
- Generic Alternatives: Your insurer might prefer a less expensive generic alternative. Your physician needs to justify why Cialis is the most suitable medication for your specific case.
- Prior Authorization History: Past denials can influence future approvals. Address previous denial reasons directly in your new application.
- Incorrect Diagnosis Codes: Using inaccurate diagnosis codes can lead to automatic rejection. Verify the codes align precisely with your patient’s condition.
- Form Errors: Errors in filling out the form itself can lead to delays. Carefully read instructions and use the correct form.
Steps to Minimize Delays
- Submit a complete application: Ensure all required fields are accurately completed.
- Provide comprehensive medical documentation: Thoroughly explain the patient’s condition and the reasons why Cialis is necessary.
- Follow up on applications: Regularly check the status of your application and contact your insurer or pharmacy if there are any delays.
- Appeal denials: If your application is denied, carefully review the denial reason and prepare a strong appeal with additional supporting documentation.
- Consult with your physician: Discuss any potential issues before submitting the application. They can help address potential problem areas proactively.
Specific Documentation to Include
To expedite the process, include these in your application:
- Detailed patient medical history relevant to Cialis use
- Results of relevant medical tests
- Documentation showing failure of alternative treatments
- Physician’s statement clearly explaining why Cialis is medically necessary
By addressing these potential issues and preparing a thorough application, you can significantly reduce the likelihood of delays and denials.
Appealing a Denied Cialis Prior Authorization Request
Review the denial letter carefully. Identify the specific reason for the denial. This is your starting point.
Gather supporting medical documentation. Include your doctor’s detailed rationale for prescribing Cialis, relevant medical records, and any lab results supporting the diagnosis. Clearly demonstrate medical necessity.
Contact your insurance provider’s prior authorization department. Request a specific contact person. Clearly state your intent to appeal and ask for clarification on any unmet requirements.
Prepare a concise, well-organized appeal letter. Address the specific reasons for denial point-by-point. Provide all supporting documentation. Maintain a professional yet persuasive tone.
Follow up on your appeal. If you don’t receive a response within a reasonable timeframe (check your insurer’s guidelines), call again. Document all communication.
Consider your next steps. If the appeal is unsuccessful, explore alternative treatments or discuss options with your doctor. You may want to consult a patient advocate for assistance.
Remember: Meticulous documentation and clear communication significantly improve your chances of a successful appeal.
Note: This information is for guidance only and does not constitute medical or legal advice. Always consult with your healthcare provider and insurance company for specific details.
Alternative Medications and Cost-Saving Strategies If Cialis is Denied
Consider Tadalafil, the generic version of Cialis. It offers the same active ingredient at a significantly lower cost. Explore pharmacies that offer generic medications or use online prescription services for potential price comparisons.
Other PDE5 Inhibitors
Explore alternative PDE5 inhibitors like Viagra (sildenafil) or Levitra (vardenafil). Each medication has a slightly different profile, and one might be better suited to your needs. Discuss these options with your doctor to determine the best fit.
Negotiate with your insurance provider. Appeal the prior authorization decision, providing additional medical information if necessary. Sometimes, a simple phone call can resolve issues.
Explore manufacturer patient assistance programs. Pharmaceutical companies often offer financial assistance for their medications. Check the websites of Lilly (Cialis) and other manufacturers for details.
Lifestyle Changes and Alternative Approaches
Improve your overall health. Regular exercise, a healthy diet, and stress reduction techniques can positively impact erectile function. This can reduce reliance on medication or enhance its effectiveness.
Counseling. Consider couples or individual therapy to address psychological factors contributing to erectile dysfunction. This approach can be incredibly helpful.
Consult with your doctor. Discuss your financial constraints openly with your physician. They may be able to suggest additional strategies or alternative treatment options.